Summary
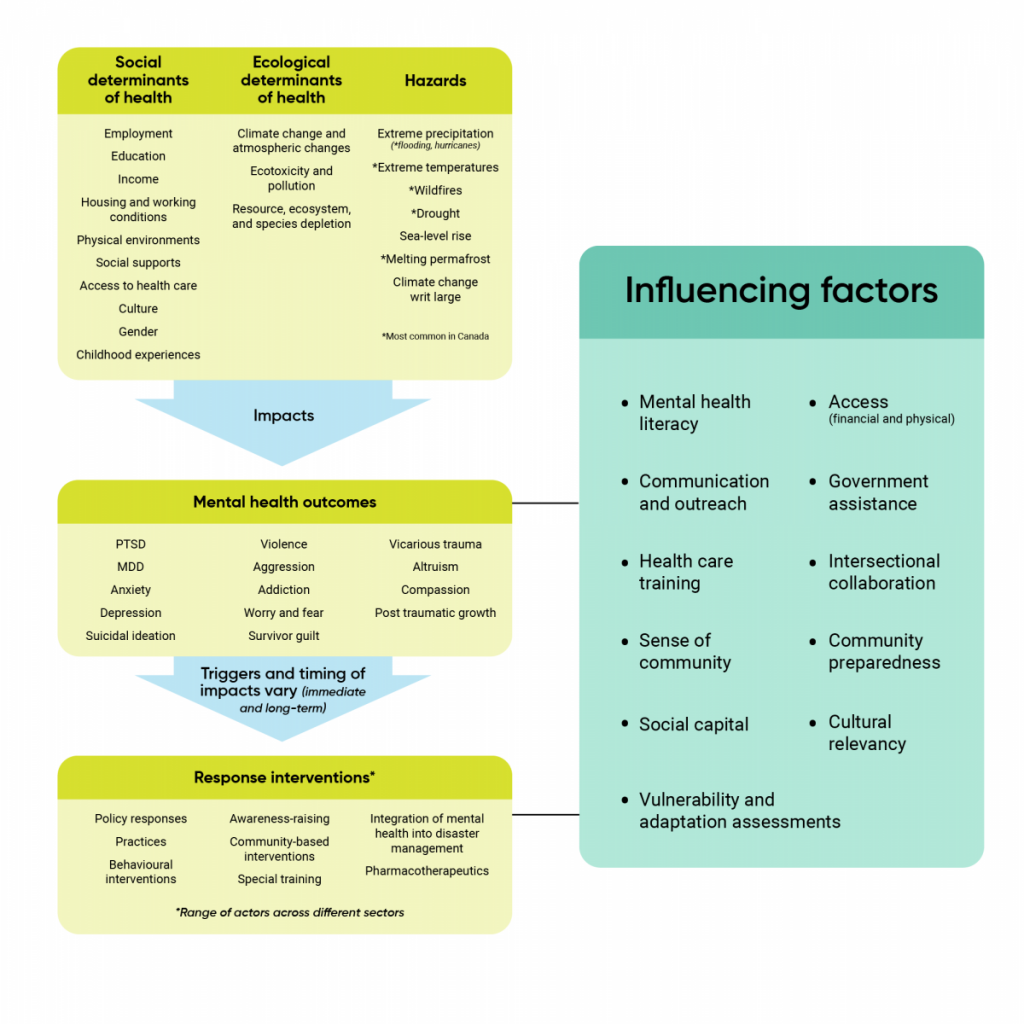
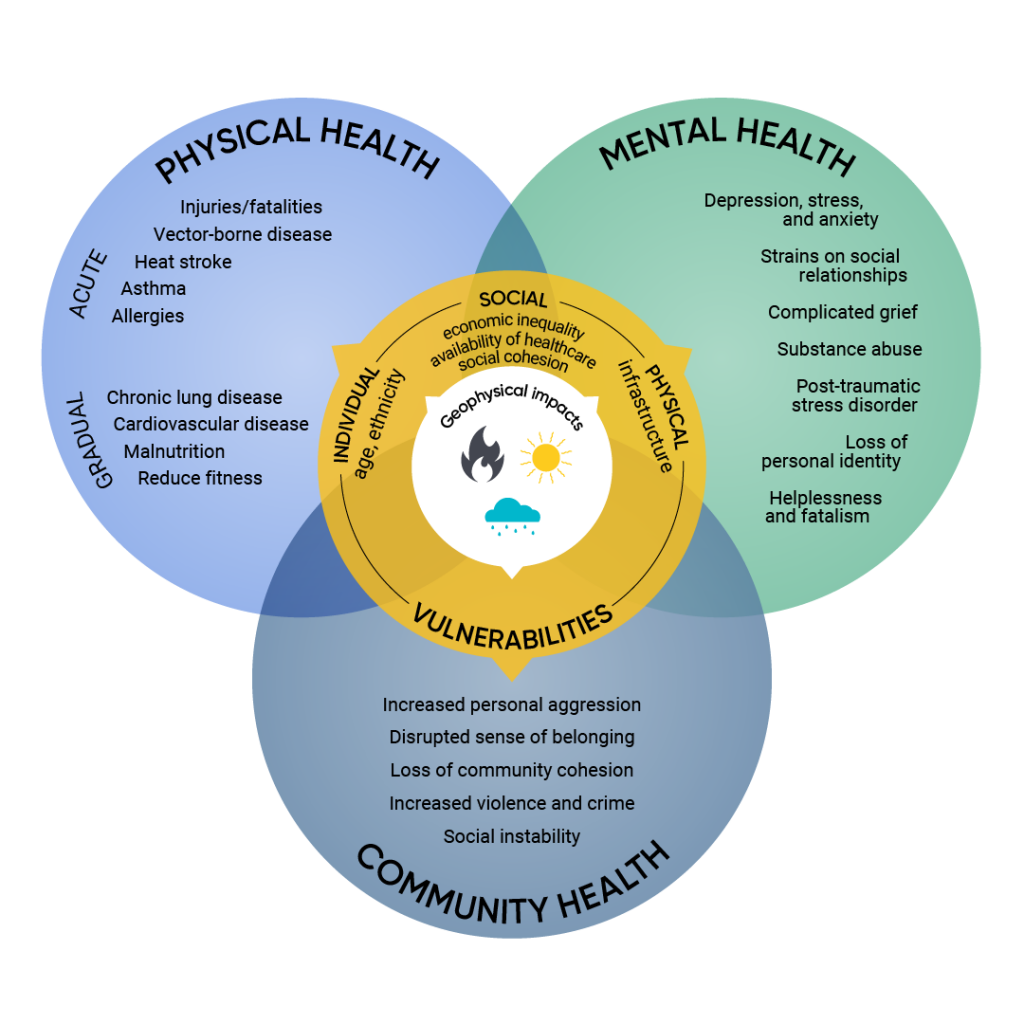
Climate change increases risks to the mental health and well-being of many people in Canada. Specific populations that can be disproportionally and inequitably affected include those experiencing health inequities based on race, culture, gender, age, socio-economic status, ability, and geographic location. These factors are encompassed within the social, biological, environmental, and cultural determinants of health that are amplified by climate change. Mental health can be impacted by hazards that occur over the shorter and longer term, such as floods, extreme heat events, wildfires, and hurricanes as well as drought, sea-level rise, and melting permafrost. Knowledge and awareness of climate change threats can also affect mental health and well-being, resulting in emotional and behavioural responses, such as worry, grief, anxiety, anger, hopelessness, and fear.
Mental health impacts of climate change may include exacerbation of existing mental illness such as psychosis; new-onset mental illness such as post-traumatic stress disorder; mental health stressors such as grief, worry, anxiety, and vicarious trauma; and a lost sense of place, which refers to the perceived or actual detachment from community, environment, or homeland. Impacts can also include disruptions to psychosocial well-being and resilience, disruptions to a sense of meaning in a person’s life, and lack of community cohesion, all of which can result in distress, higher rates of hospital admissions, increased suicide ideation or suicide, and increased negative behaviours such as substance misuse, violence, and aggression. Adaptation efforts that can reduce the mental health impacts of climate change include expanded communication and outreach activities and community preparedness, greater access to health care for those requiring assistance, and improved mental health literacy and training.
Key Messages
- The current burden of mental ill health in Canada is likely to rise as a result of climate change. Given the very large number of Canadians who experience mental health problems, the potential increase of mental ill health outcomes from future climate change is large.
- Climate change hazards that can affect the mental health of people in Canada include acute hazards such as floods, extreme heat events, wildfires, and hurricanes, as well as slow-onset hazards such as drought, sea-level rise, and melting permafrost. Secondary impacts of climate hazards (such as economic insecurity, displacement, food and water insecurity) can lead to ongoing stress, anxiety, and depression.
- Mental health impacts of climate change may include exacerbation of existing mental illness such as psychosis; new-onset mental illness such as post-traumatic stress disorder; mental health stressors such as grief, worry, anxiety, and vicarious trauma; and a lost sense of place, which refers to the perceived or actual detachment from community, environment, or homeland. Impacts can also include disruptions to psychosocial well-being and resilience, disruptions to a sense of meaning in a person’s life, and lack of community cohesion, all of which can result in distress, higher rates of hospital admissions, increased suicide ideation or suicide, and increased negative behaviours such as substance misuse, violence, and aggression.
- Climate change and related environmental change can cause complex emotional and behavioural reactions in individuals, that are not necessarily pathological. These environmental distress reactions, called psychoterratic syndromes, include ecoanxiety, solastalgia, and ecoparalysis.
- Climate change disproportionately affects the mental health of specific populations, including Indigenous Peoples; women; children; youth; older adults; people living in low socio-economic conditions (including the homeless); people living with pre-existing physical and mental health conditions; and certain occupational groups, such as land-based workers and first responders. For example, Indigenous Peoples are at greater risk of being displaced by climate-related hazards and this can result in a loss of community connections and loss of livelihoods that affect individual and collective well-being.
- Given the current high costs of mental illness to society, and the breadth of mental health impacts that are related to climate change, future costs borne by Canadians and health systems are expected to be large as the climate continues to warm.
- Access to mental health practitioners, mental health and health care facilities, social services, and culturally relevant mental health care information can prevent adverse mental health outcomes, improve outcomes, and enhance well-being in a changing climate. Rural, remote, and urban settings that currently face challenges providing mental health care will face increased demands for services from climate change impacts.
- Greater communication and outreach about the mental health impacts of climate change, enhanced community preparedness for possible impacts, broad access to culturally relevant health care to assist people in need, intersectoral and transdisciplinary collaboration on adaptation initiatives, and improved mental health literacy and training support efforts to prepare for climate change impacts on Canadians.
- Well-designed actions to mitigate greenhouse gas emissions and adapt to climate change — for example, active transportation, environmental stewardship, green infrastructure, and enhanced social networks and community supports — can also benefit mental health.
Figure 4.2
Factors that influence the psychosocial health impacts of climate change.
Source
Hayes et al., 2019.
Overview of Climate Change Impacts on Mental Health
| Health Impact or Hazard Category | Climate-Related Causes | Possible Health Effects |
| Mental health |
|
|